we are here to fit your needs
We are experienced in offering medical billing and coding support for individual physicians, physician groups, free standing diagnostic facilities, multi-specialty groups, clinics, long-term care facilities, acute care facilities, and hospitals. We create, submit, follow-up and post surgery medical claims within the same day.
Our medical billing services for general surgery practice cover:
Charge entry on a daily basis
Review of all charges for completeness and accuracy
ERA and EOB payment posting on a daily basis
Double checking of claims and claims scrubbing before submission
Identification and handling of secondary balances and patient responsibility
Comprehensive claim and AR follow-up
Special focus on denied claims
You can decide between your own billing software or one of our suppporting software vendors.
Our claim scrubbing process verifies and validates all patient information, CPT/ICD9, HCPCS code combinations, instantly checks the codes against National Correct Coding Initiatives (CCI) edits, Medically Unlikely Edits (MUEs), and frequency allowances.
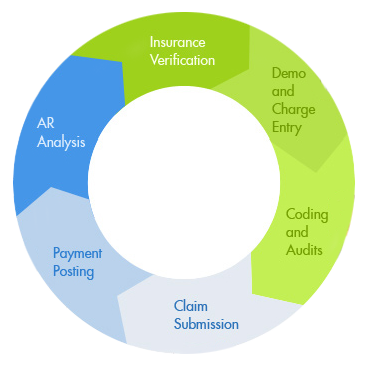
Our Process
Three major components to succesful billing.
Charge Entry
The billing process begins with filing claims for services provided, entering charges/ creating bills is done electronically to shorten the revenue cycle.
Payment Posting
Payment posting is a critical part of the billing process, we are efficient and accurate when handling a paymnet posting account.
Account Receivables
We aim to increase our clients cash flow by limiting the days in accounts receivable and improving profitabilty.
Verifies the patients insurance details.
Enters the patient's personal information from the demographic sheets.
Assigns numerical codes for CPT and the diagnosis code. Entries chedcked for accuracy based on carrier requirements.
The audited medical claims are submitted and followed up to insurance companies.
Applies the payments into the billing software against the appropriate patient account.
Claim problems are identified and resolved for the payment of the claim.